LONDON, UK – July 17, 2025
Three-Parent Baby – In a monumental leap for reproductive medicine, British researchers have announced the successful birth of eight healthy babies using a groundbreaking IVF technique that combines DNA from three individuals. This pioneering procedure, known as Mitochondrial Donation Treatment (MDT), offers a lifeline to mothers at risk of passing on devastating, incurable genetic diseases to their children. This was the intention i.e. to avoid genetic diseases in children.
The news, published today in the esteemed New England Journal of Medicine, confirms the success of a world-first trial. It solidifies the UK’s position at the forefront of ethical and regulated applications of advanced genetic technologies, bringing immense hope to families previously facing heartbreak.
Table of Contents
What’s a three-parent baby?
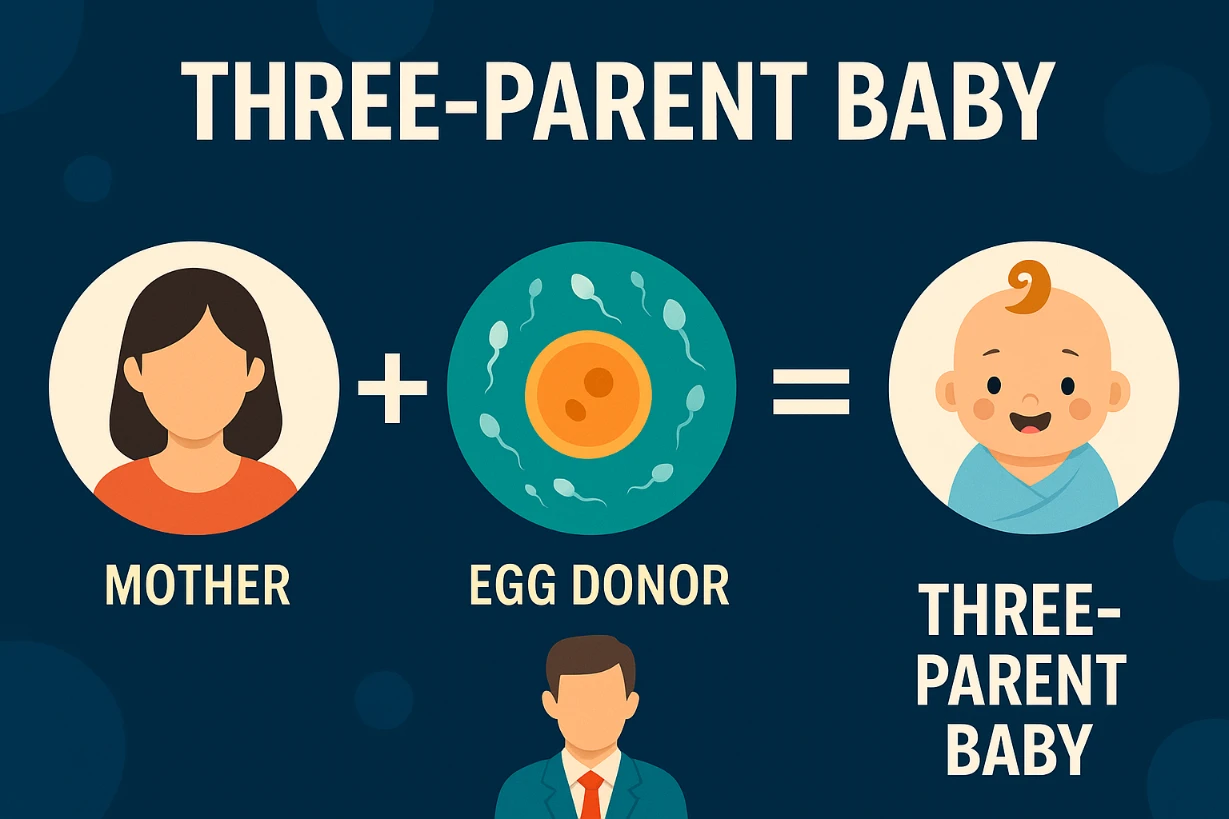
A three-parent baby is a child born using a special form of in vitro fertilization (IVF) that involves DNA from three people:
- Mother (provides the nucleus of the egg)
- Father (provides the sperm)
- Donor woman (provides a healthy egg with working mitochondria)
How the “Three-Parent Baby” Method Works
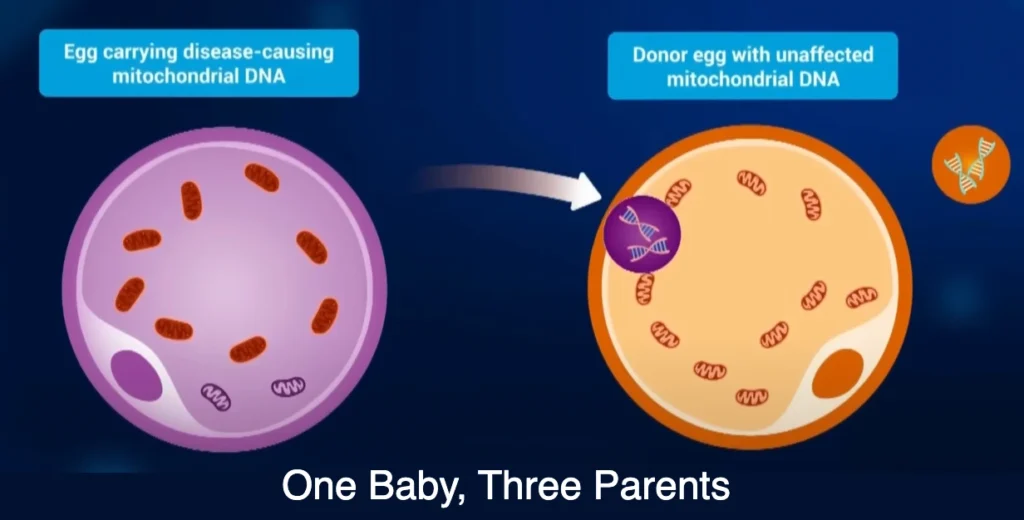
Mitochondrial diseases are severe conditions caused by faulty genes in the mitochondria, the tiny powerhouses within our cells responsible for energy production. These diseases, which can affect vital organs like the brain, heart, and muscles, are inherited directly from the mother.
MDT, sometimes controversially called the “three-parent baby” technique, prevents this inheritance by:
- Using the mother’s nuclear DNA: This is the main genetic material that defines a child’s unique traits (e.g., hair color, personality) and comes from the biological mother’s egg.
- Utilizing a healthy donor egg: A donor woman provides an egg with healthy mitochondria, but its own nuclear DNA is removed.
- Creating a new egg: The biological mother’s healthy nuclear DNA is then transferred into the donor’s “empty” egg, which now contains healthy mitochondria.
- Fertilization: This newly constructed egg is then fertilized with the father’s sperm, and the resulting embryo is implanted into the mother.
The baby inherits virtually all of its genetic traits (over 99.8% of its DNA) from its biological mother and father, with only a tiny fraction (around 0.02%) of mitochondrial DNA coming from the donor. This small amount of donor DNA does not influence physical appearance or personality.
A Decade of Progress: From Law to Lives Changed
Britain became the first country to legally approve mitochondrial donation in 2015, following extensive ethical and scientific reviews. The Newcastle Fertility Centre in northeast England became the pioneering clinic licensed to perform the procedure, with the first cases approved in 2018.
Of the 22 women who underwent the treatment at the Newcastle centre, eight healthy babies have been born to seven women. These four boys and four girls, including one set of identical twins, range in age from under six months to over two years old. Researchers confirmed that the amount of mutated mitochondrial DNA was reduced by 95-100% in six babies, and by 77-88% in the other two – levels well below what causes disease. While three babies showed some early, non-MDT related health issues that were successfully treated, all eight are currently healthy and meeting their developmental milestones.
The Human Fertilisation and Embryology Authority (HFEA), the UK’s independent regulator for fertility treatment, has overseen the strict approval process, ensuring that only individuals with a “very high risk” of passing on a serious mitochondrial disease are eligible. As of July 1, 2025, 35 patients have been approved for the treatment.
Now, let’s understand the “good” and “bad” of this:
Three-Parent Babies – The Good (Advantages/Benefits):
- Prevents Devastating Mitochondrial Diseases: This is the primary and most significant advantage. For women who carry severe mitochondrial DNA (mtDNA) mutations, MDT offers the only known way to have a genetically related child who will not inherit these debilitating and often fatal conditions. These diseases can cause severe neurological problems, muscle weakness, heart failure, and more.
- Offers a Family Planning Option: Without MDT, couples at high risk of passing on mitochondrial disease would typically only have options like adoption, using donor eggs (which means the child would not be genetically related to the mother), or not having children. MDT allows them to have a child with the nuclear DNA of both biological parents.
- Maintains Genetic Link to Both Parents: The child receives almost all of its genetic material (over 99.8%) from the intended mother and father, preserving their unique genetic lineage. Only the tiny fraction of mitochondrial DNA comes from the donor.
- Reduces Suffering: By preventing the transmission of severe diseases, MDT can save children from immense suffering and often premature death, improving their quality of life dramatically.
- Pioneering Medical Advancement: The success of MDT pushes the boundaries of reproductive medicine and genetics, potentially paving the way for future therapies that address other genetic conditions.
- Healthy Outcomes (So Far): As seen with the eight healthy babies born in the UK, the procedure has proven effective in reducing the mutant mitochondrial DNA to non-disease-causing levels, with the children meeting developmental milestones.
Three-Parent Babies – The Bad (Disadvantages/Concerns/Ethical Debates):
- Ethical Concerns about “Designer Babies” and Germline Editing:
- “Three Genetic Parents”: The term itself sparks debate. While the donor contributes a tiny fraction of DNA that doesn’t influence traits, critics argue it technically means a child has DNA from three people, which some find ethically problematic or “unnatural.”
- Germline Modification: This technique results in a heritable genetic change – the healthy mitochondrial DNA from the donor is passed down to future generations (if the baby is a girl). This is a form of germline editing, which many countries prohibit due to concerns about unintended long-term consequences that cannot be reversed.
- Slippery Slope Argument: Critics worry that if MDT is allowed, it could open the door to “designer babies” – using similar techniques to select for non-medical traits like intelligence, appearance, or athletic ability, leading to eugenics. Proponents counter that MDT is solely for preventing disease, not enhancing traits.
- Safety and Unforeseen Risks:
- Long-Term Unknowns: While the initial results are promising, the long-term health and developmental outcomes for these children, and potentially their offspring, are still unknown. The technology is relatively new, and comprehensive long-term follow-up studies are crucial.
- Mitochondrial “Carryover” or “Reversion”: It’s not always possible to completely eliminate the mother’s faulty mitochondria during the transfer. There’s a small risk that residual faulty mitochondria from the biological mother could multiply over time in the child, potentially leading to disease symptoms later in life (a phenomenon known as “reversion” or “heteroplasmy reversal”). The UK study did find some low levels of maternal mtDNA in some babies, which need continued monitoring.
- Compatibility Issues: Though not strongly evidenced in humans, some animal studies have shown potential incompatibility issues between the donor’s mitochondria and the recipient’s nuclear DNA, leading to metabolic problems.
- Impact on Identity:
- Some ethicists and individuals question how a child might feel about having a genetic contribution from a third person, even if it’s very small. Will it affect their sense of identity or lineage?
- Egg Donor Risks and Exploitation:
- The procedure requires a healthy egg donor, who must undergo hormone stimulation and egg retrieval, which carries physical risks (e.g., Ovarian Hyperstimulation Syndrome) and ethical concerns around compensation and potential exploitation, particularly if demand increases.
- Embryo Creation and Destruction:
- The Pronuclear Transfer (PNT) method involves fertilizing two eggs (mother’s and donor’s) and then discarding parts of the donor’s fertilized egg, which raises ethical concerns for those who believe life begins at conception and object to embryo destruction.
Hope Amidst Ongoing Discussion
This success offers immense hope to families who previously had no option for a genetically related child free from these debilitating diseases. As one mother stated, “After years of uncertainty, this treatment gave us hope — and then it gave us our baby. Science gave us a chance.”
While the technique is now also permitted in countries like Australia, it remains controversial and unapproved in many others, including the United States, due to ethical concerns. However, proponents argue that the overwhelming benefit of preventing severe suffering far outweighs the minimal genetic contribution from a third party.
The diligent monitoring of these children will continue, providing invaluable long-term data. This breakthrough not only transforms the lives of affected families but also pushes the boundaries of genetic medicine, setting a precedent for future innovations in preventing inherited diseases.
Keep following Duniya Daily for more such interesting news and updates!